
Tìm Kiếm Bài Đã Đăng

In early September of 2014, on the Health section of The New York Times, reporter Anahad O’Connor published an article with the title “A Call for a Low-Carb Diet That Embraces Fat”.
<https://www.nytimes.com/2014/09/02/health/low-carb-vs-low-fat-diet.html?_r=0>
This article marked an important change of direction among the media and the American public at large in their view of nutrition from a fat avoidance to embracing more fat in their diet. In it O’Connor seeks to inform his readers of new solid scientific evidence indicating a diet low in carbohydrates and higher in fat (except Trans-fat) can significantly decrease cardio-vascular disease risk and promote weight loss by ridding the body of fatty tissue as demonstrated in the results of the latest clinical study from Tulane University supported by a grant from the National Institute of Health and published in the Annals of Internal Medicine. It was a well designed prospective control study which clearly showed the Low-Carb More-Fat study group ended up with more weight loss and better cholesterol levels than the Low-Fat Diet group, who consumed their food according to the current guideline from the US Government and supported by the American Heart Association. It is interesting to note that neither the study group nor the control group had to limit their calorie intake, unlike most other diet and nutrition studies before. These results indicate that the low fat approach to diet in the USA during the past 30 years is not valid for public health.
How did it happen?
It has been known since the 1950s that a high level of serum cholesterol is a major risk factor for cardio-vascular disease, but where that cholesterol came from remained uncertain. Cholesterol plays a vital role in cellular structure and also in the chemical scaffold of the all important steroid hormones and the production of vitamin D within the body. In the 1960s, medical research discovered a few rare genetic diseases which raise the levels of blood lipids (cholesterol, triglyceride etc…); however, in most patients with cardio-vascular disease the cholesterol in their blood appeared to be related to their dietary intake.
A contentious academic battle exploded between medical scientists who believed that patients with high blood lipid levels got those elevated levels from excessive consumption of sugar and other carbohydrates and other colleagues who believed that those lipids in the serum came from eating fatty food. Finally, in the 1970s, Dr. Ancel Keys from the Division of Medical Nutrition at the University of Minnesota, presented his findings of the important Seven Nation (European and American) Study which purportedly showed that consuming saturated animal fat led to high serum cholesterol and cardiovascular disease. Other scientists quickly supported Keys’ results, and the American Heart Association as well as the US Government advised Americans to eat less fat, especially animal fat. The food industry was encouraged to reduce the amount of fat in products before they hit the supermarket shelves.
Tragic consequence and paradoxes:
American consumers have been bombarded with big catchy Low Fat and No Fat marketing labels at the grocery stores. To replace the butter which Americans loved to spread on their bread but now were told was unhealthful, food scientists came up with a way to harden vegetable oil by hydrogenising the old liquid vegetable fat with the Trans bond; the so called vegetable Trans-fat was born as vegetable margarine which was marketed as a healthier alternative to butter. Vegetable Trans-fat does not exist in nature and now has been shown to be a very unhealthful fat for human consumption.
From the 1980s until the present time, the US and other prosperous industrialized countries have experienced an epidemic of obesity and Type 2 Diabetes. A significant number of the adult population suffers from Metabolic Syndrome as a result of insulin resistance at the tissue level-which causes adiposity, hyperlipidemia (high cholesterol and triglyceride blood levels), high blood pressure and Type 2 Diabetes. During the last 7-8 years, medical researchers have been able to pinpoint the cause of this epidemic: Americans have consumed excessive amounts of carbohydrates to make up for the missing calories (and taste) from eating less fat. Sugar, especially fructose, the sweetest sugar, is extremely adipogenic, which causes fat infiltration in the liver and abdomen as well as in skeletal muscles and leads to tissue insulin resistance (after tissue insulin resistance occurs, glucose will become harmful as well). Furthermore, fructose can decrease satiety which is a cause of overeating-which aggravates obesity. American consumers have paid a high price with their health and their lives for consuming those Low Fat and No Fat products presented to them as healthful food choices. Meanwhile, their physicians continue to advise them erroneously to avoid fat, particularly animal fat.
Several paradoxes occurred during this long period of time which somehow were not noticed by medical scientists and the US Government for any serious consideration because the authorities still deeply believed in the Low Fat doctrine.
1-The French paradox: French people revere their culinary standards for taste and therefore refused to go Low Fat and continued cooking using butter to serve beef, pork, poultry and sea food dishes on their dinner table. Yet, the French rate of obesity, diabetes and cardio-vascular disease has remained lower than their Western European and US counterparts. This paradox was credited to the French higher consumption of red wine which contains resveratrol.
2-The anti-cholesterol drugs paradox: The FDA approved 6 groups of cholesterol (and lipid) lowering drugs to be sold in the US- but only one group, the statins have been shown in clinical use to help prevent cardio-vascular disease and its complications and extend longevity of patients. All other groups failed to help patients improve their outcomes although their blood lipid levels got lowered with the drugs.
3-The diabetic complications paradox: Despite the worsening of the Type 2 Diabetes epidemic (with potential for serious cardio-vascular complications) the rate and mortality of heart attack and stroke have declined in the US for the last 15 years because American physicians have been diligent in prescribing anti-hypertensive medications and statin drugs to their patients.
Thanks to the study from Tulane University and O’Connor’s NY Times article, we have realized that the above “paradoxes” were not paradoxical at all. American medicine and the US government were simply wrong to have promoted the fat depleted diet to its people. The 7 Nation Study of Professor Keys has recently been scrutinized by other scientists and found to have many flaws in methodology that led to erroneous conclusion about dietary fat and blood cholesterol.
Eating little fat causes deficiencies in fat soluble vitamins (A, D, K and E) with detrimental effects on health.
Diet too low in fat, particularly animal fat, has been linked to parenchymal brain hemorrhage after age 45 in several studies involving American nurses (2001), Japanese men (2003) and people living in India (2012). The Zen master Thich Nhat Hanh suffered from brain hemorrhage recently; one wonders if his age and diet devoid of animal fat could have been the risk factors as reported in the studies cited above.
We should also be aware that several types of cancer occur frequently in patients with very low levels of serum cholesterol. To this day, however, medical science hasn’t shown whether very low cholesterol is a risk factor for cancer-or if cancer itself causes the level of cholesterol to drop.
Conclusion:
Americans still follow the Low Fat dietary guideline promoted by their government with a goal of fat amounting to 30% or less of the total daily calorie intake and therefore consume too much sugar and starch (carbohydrates) with bad consequences to their health. First Lady Michelle Obama promotes a policy in which public school cafeterias serve only low sugar low fat food to the students which has led to lunch that tastes so bland and unappetizing (like cardboard) that many students have complained and even refused to eat their cafeteria food. Many cardiologists still push for a “heart healthy” diet with only 10% of calories coming from fat although such a diet will increase the risk of brain hemorrhage. However the latest research, cited at the beginning of this article, demonstrated that consuming a diet with fat accounting for 40% or more of total calorie intake while eating fewer carbohydrates led to weight loss with satiety and improved cardio-vascular risk parameters.
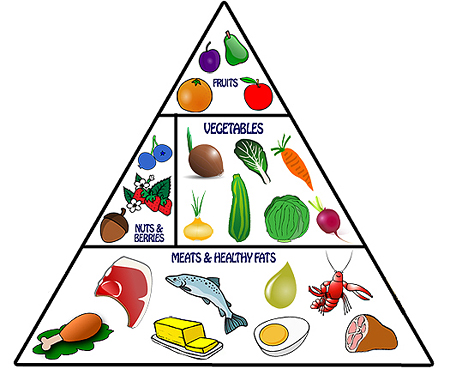
We should enjoy eating our food rich in protein and fat-such as beef, pork, poultry, eggs and seafood- without fear. We should also eat fewer carbohydrates and avoid processed sugar - eating more fruits and vegetable instead. When shopping for groceries, we should not buy those with Low Fat or No Fat on the labels and we should absolutely stay away from vegetable Trans-fat which is the only type of fat proved to be dangerous and unfit for human consumption.
The good fats are mono-unsaturated fat and omega-3-fatty acid because they provide anti-inflammation benefits and prevent cardio-vascular disease. Good fat can be found in olive oil, canola oil, fish liver oil, avocados, duck fat, coconut oil, peanut oil, egg yolks and many more foods….. Saturated fat from beef, pork or poly-unsaturated fat from soy, corn, etc… is harmless if not over consumed. People who eat lots of fish or poultry have lower risk of stroke, while those who consume little fat end up with higher risk for bleeding in the brain, as reported in scientific studies.
Pham H. Liem, MD
Former Jackson T. Stephens Professor and Vice-Chairman of the Donald W. Reynolds Department of Geriatrics, UAMS
<https://www.nytimes.com/2014/09/02/health/low-carb-vs-low-fat-diet.html?_r=0>
This article marked an important change of direction among the media and the American public at large in their view of nutrition from a fat avoidance to embracing more fat in their diet. In it O’Connor seeks to inform his readers of new solid scientific evidence indicating a diet low in carbohydrates and higher in fat (except Trans-fat) can significantly decrease cardio-vascular disease risk and promote weight loss by ridding the body of fatty tissue as demonstrated in the results of the latest clinical study from Tulane University supported by a grant from the National Institute of Health and published in the Annals of Internal Medicine. It was a well designed prospective control study which clearly showed the Low-Carb More-Fat study group ended up with more weight loss and better cholesterol levels than the Low-Fat Diet group, who consumed their food according to the current guideline from the US Government and supported by the American Heart Association. It is interesting to note that neither the study group nor the control group had to limit their calorie intake, unlike most other diet and nutrition studies before. These results indicate that the low fat approach to diet in the USA during the past 30 years is not valid for public health.
How did it happen?
It has been known since the 1950s that a high level of serum cholesterol is a major risk factor for cardio-vascular disease, but where that cholesterol came from remained uncertain. Cholesterol plays a vital role in cellular structure and also in the chemical scaffold of the all important steroid hormones and the production of vitamin D within the body. In the 1960s, medical research discovered a few rare genetic diseases which raise the levels of blood lipids (cholesterol, triglyceride etc…); however, in most patients with cardio-vascular disease the cholesterol in their blood appeared to be related to their dietary intake.
A contentious academic battle exploded between medical scientists who believed that patients with high blood lipid levels got those elevated levels from excessive consumption of sugar and other carbohydrates and other colleagues who believed that those lipids in the serum came from eating fatty food. Finally, in the 1970s, Dr. Ancel Keys from the Division of Medical Nutrition at the University of Minnesota, presented his findings of the important Seven Nation (European and American) Study which purportedly showed that consuming saturated animal fat led to high serum cholesterol and cardiovascular disease. Other scientists quickly supported Keys’ results, and the American Heart Association as well as the US Government advised Americans to eat less fat, especially animal fat. The food industry was encouraged to reduce the amount of fat in products before they hit the supermarket shelves.
Tragic consequence and paradoxes:
American consumers have been bombarded with big catchy Low Fat and No Fat marketing labels at the grocery stores. To replace the butter which Americans loved to spread on their bread but now were told was unhealthful, food scientists came up with a way to harden vegetable oil by hydrogenising the old liquid vegetable fat with the Trans bond; the so called vegetable Trans-fat was born as vegetable margarine which was marketed as a healthier alternative to butter. Vegetable Trans-fat does not exist in nature and now has been shown to be a very unhealthful fat for human consumption.
From the 1980s until the present time, the US and other prosperous industrialized countries have experienced an epidemic of obesity and Type 2 Diabetes. A significant number of the adult population suffers from Metabolic Syndrome as a result of insulin resistance at the tissue level-which causes adiposity, hyperlipidemia (high cholesterol and triglyceride blood levels), high blood pressure and Type 2 Diabetes. During the last 7-8 years, medical researchers have been able to pinpoint the cause of this epidemic: Americans have consumed excessive amounts of carbohydrates to make up for the missing calories (and taste) from eating less fat. Sugar, especially fructose, the sweetest sugar, is extremely adipogenic, which causes fat infiltration in the liver and abdomen as well as in skeletal muscles and leads to tissue insulin resistance (after tissue insulin resistance occurs, glucose will become harmful as well). Furthermore, fructose can decrease satiety which is a cause of overeating-which aggravates obesity. American consumers have paid a high price with their health and their lives for consuming those Low Fat and No Fat products presented to them as healthful food choices. Meanwhile, their physicians continue to advise them erroneously to avoid fat, particularly animal fat.
Several paradoxes occurred during this long period of time which somehow were not noticed by medical scientists and the US Government for any serious consideration because the authorities still deeply believed in the Low Fat doctrine.
1-The French paradox: French people revere their culinary standards for taste and therefore refused to go Low Fat and continued cooking using butter to serve beef, pork, poultry and sea food dishes on their dinner table. Yet, the French rate of obesity, diabetes and cardio-vascular disease has remained lower than their Western European and US counterparts. This paradox was credited to the French higher consumption of red wine which contains resveratrol.
2-The anti-cholesterol drugs paradox: The FDA approved 6 groups of cholesterol (and lipid) lowering drugs to be sold in the US- but only one group, the statins have been shown in clinical use to help prevent cardio-vascular disease and its complications and extend longevity of patients. All other groups failed to help patients improve their outcomes although their blood lipid levels got lowered with the drugs.
3-The diabetic complications paradox: Despite the worsening of the Type 2 Diabetes epidemic (with potential for serious cardio-vascular complications) the rate and mortality of heart attack and stroke have declined in the US for the last 15 years because American physicians have been diligent in prescribing anti-hypertensive medications and statin drugs to their patients.
Thanks to the study from Tulane University and O’Connor’s NY Times article, we have realized that the above “paradoxes” were not paradoxical at all. American medicine and the US government were simply wrong to have promoted the fat depleted diet to its people. The 7 Nation Study of Professor Keys has recently been scrutinized by other scientists and found to have many flaws in methodology that led to erroneous conclusion about dietary fat and blood cholesterol.
Eating little fat causes deficiencies in fat soluble vitamins (A, D, K and E) with detrimental effects on health.
Diet too low in fat, particularly animal fat, has been linked to parenchymal brain hemorrhage after age 45 in several studies involving American nurses (2001), Japanese men (2003) and people living in India (2012). The Zen master Thich Nhat Hanh suffered from brain hemorrhage recently; one wonders if his age and diet devoid of animal fat could have been the risk factors as reported in the studies cited above.
We should also be aware that several types of cancer occur frequently in patients with very low levels of serum cholesterol. To this day, however, medical science hasn’t shown whether very low cholesterol is a risk factor for cancer-or if cancer itself causes the level of cholesterol to drop.
Conclusion:
Americans still follow the Low Fat dietary guideline promoted by their government with a goal of fat amounting to 30% or less of the total daily calorie intake and therefore consume too much sugar and starch (carbohydrates) with bad consequences to their health. First Lady Michelle Obama promotes a policy in which public school cafeterias serve only low sugar low fat food to the students which has led to lunch that tastes so bland and unappetizing (like cardboard) that many students have complained and even refused to eat their cafeteria food. Many cardiologists still push for a “heart healthy” diet with only 10% of calories coming from fat although such a diet will increase the risk of brain hemorrhage. However the latest research, cited at the beginning of this article, demonstrated that consuming a diet with fat accounting for 40% or more of total calorie intake while eating fewer carbohydrates led to weight loss with satiety and improved cardio-vascular risk parameters.
We should enjoy eating our food rich in protein and fat-such as beef, pork, poultry, eggs and seafood- without fear. We should also eat fewer carbohydrates and avoid processed sugar - eating more fruits and vegetable instead. When shopping for groceries, we should not buy those with Low Fat or No Fat on the labels and we should absolutely stay away from vegetable Trans-fat which is the only type of fat proved to be dangerous and unfit for human consumption.
The good fats are mono-unsaturated fat and omega-3-fatty acid because they provide anti-inflammation benefits and prevent cardio-vascular disease. Good fat can be found in olive oil, canola oil, fish liver oil, avocados, duck fat, coconut oil, peanut oil, egg yolks and many more foods….. Saturated fat from beef, pork or poly-unsaturated fat from soy, corn, etc… is harmless if not over consumed. People who eat lots of fish or poultry have lower risk of stroke, while those who consume little fat end up with higher risk for bleeding in the brain, as reported in scientific studies.
Pham H. Liem, MD
Former Jackson T. Stephens Professor and Vice-Chairman of the Donald W. Reynolds Department of Geriatrics, UAMS

Diễn Đàn Cựu Sinh Viên Quân Y
© 2015
© 2015
Loading